Living with Osteoporosis: What To Do For Better Bone Health
Article by Anna Kania
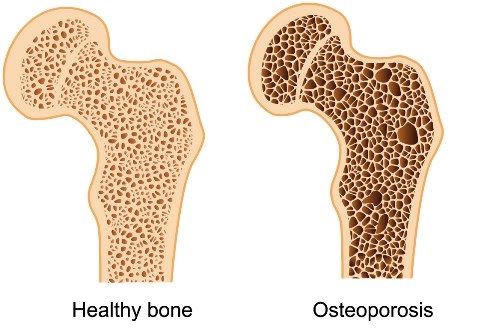
Osteoporosis is a disease characterized by low bone mass and deterioration of bone tissue, which can lead to increased risk of fracture.

The most common fractures associated with osteoporosis are in the hip, spine, wrist and shoulder.
Prevalence of osteoporosis
While Osteoporosis can affect people at any age, it is most common among people 50 years of age or older.
- 2 million Canadians are affected by osteoporosis
- At least 1 in 3 women and 1 in 5 men will break a bone due to osteoporosis in their lifetime
- Fragility fractures represent 80% of all fractures in menopausal women over the age of 50
- Fractures from osteoporosis are more common than heart attack, stroke and breast cancer combined
Diagnosis: bone densitometry
The most common bone density test in use today is called dual energy x-ray absorptiometry (DXA). This test involves lying on a table for several minutes while a small x-ray detector scans your spine, one hip, or both. You may be asked to lift your legs onto a support to straighten your back for the test.
The test is safe and painless and does not require any injections or any other discomfort.
In BMD (Bone Mineral Density) test results, your bones are compared to the bones of an average young adult. A score (called a T-score) is calculated that describes the density of your bones in comparison to this standard.
A T-score below -2.5 indicates osteoporosis and a score between -1 and -2.5 indicates “osteopenia” or low bone density. Normal bone density is anything above -1.
Am I at risk for a fracture?
In the past 10 years, a great deal of research has identified factors other than bone mineral density that contribute to the risk of fracture.
Risk factors include:
- Being female
- After menopause
- 65+ years old
- Low calcium (< 1000mg) and vitamin D (< 2000IU) intake in your diet
- Low physical activity level ( less than 2.5 hrs per week)
- Consuming more than 3 alcohol beverages per day
- Smoking cigarettes
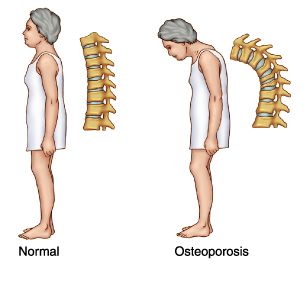
- Losing > 6cm of height from when you were a young adult
- A family history of osteoporosis or hip fracture
- History of a broken bone from a simple fall since age > 40
- Long term use of certain medications (steroids, some antidepressants, proton pump inhibitors, and others)
- Having a chronic medical condition (rheumatoid arthritis, Crohn’s disease, ulcerative collitis, celiac disease, chronic kidney or liver disease, type 1 diabetes, COPD and others),
- Early menopause < 45 years old
- Disruption of menstrual cycles; and
- A history of previous falls.
Living with osteoporosis or low bone density
If you are diagnosed with osteoporosis or low bone density it is important to focus on what you CAN do, and remember that people with osteoporosis adjust and go on to live full, active lives.
With the help of appropriate lifestyle changes and medications, you can reduce the risk of fracture.
A surprisingly effective intervention relates to reducing the risk of falls by making your home safer. Environmental changes such as making sure there’s enough light in your home, removing throw rugs and clutter that you may trip over, and putting sturdy handrails on stairs are proven to reduce the frequency of falls.
Treatment for osteoporosis or low bone density
For those living with osteoporosis, there are a variety of treatment options available. The primary goal of treatment is to prevent or slow bone loss and reduce the risk of fracture.
Specific drug treatments include:
- Bisphosphonates
- Denosumab
- Parathyroid Hormone
- Hormone Therapy
- SERMs (Selective Estrogen Receptor Modulators)
- Romosozumab
What can you do for a better bone health?
Improve your nutrition and stay active. Calcium and vitamin D are essential nutrients for proper bone health. Vitamin D helps to increase the absorption of calcium, ultimately building strong bones.
Exercises for healthy bones:
- Strength training - At least 2 x week
- Exercises for legs, arms, chest, shoulders, back
- Use body weight against gravity, bands, or weights (squat, wall push up, stated rows), 8-12 repetitions per exercise
-
Balance exercises - Every day
- Tai Chi, dancing, walking on your toes or heels
- Have a sturdy chair, counter, or wall nearby, and try (from easier to harder): shift weight from heels to toes while standing; stand heel to toe; stand on one foot; walk on a pretend line
- Posture awareness - Every day
- Gently tuck your chin in and draw your chest up slightly
- Imagine your collarbones are wings
- Spread your wings slightly without pulling your shoulders back
- Aerobic physical activity
- 10 mins or more, moderate to vigorous intensity
- You should feel like your heart is beating faster and you are breathing harder
- You might be able to talk while doing it, but not sing
If you have a spine fracture, consult a physical therapist/kinesiologist before using weights, and choose moderate, not vigorous aerobic physical activity
References
- https://osteoporosis.ca
- CMAJ. 2010 Nov 23; 182(17): 1829–1830.
- https://www.healthlinkbc.ca/health-topics/hw131419
You May Also Like...
-
 ArticleView Post
ArticleView PostStrengthening the Intrinsic Muscles of the Foot
Learn about the importance of exercising and strengthening your foot's intrinsic muscles – as well as what they are!
-
 ArticleView Post
ArticleView PostPhysiotherapy for Temporomandibular Disorders (TMD)
Do you clench your jaw, grind your teeth or bite your nails? Does this lead to clicking, cracking, locking or pain in your jaw? Physiotherapy may be able to help!
-
 ArticleView Post
ArticleView PostShould You Apply Heat or Ice to an Injury?
Heat or ice? Here we take a look at one of the most common questions we hear to determine what's most appropriate for your injury.